Atypical multisensory integration in Niemann-Pick type C disease – towards potential biomarkers
Abstract
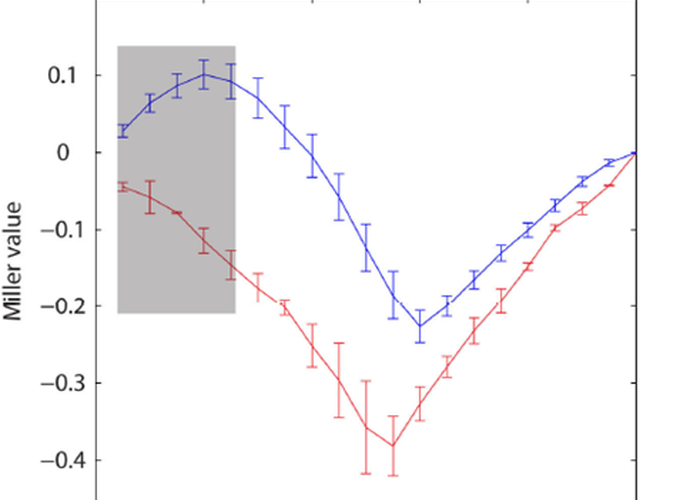
Niemann-Pick type C (NPC) is an autosomal recessive disease in which cholesterol and glycosphingolipids accumulate in lysosomes due to aberrant cell-transport mechanisms. It is characterized by progressive and ultimately terminal neurological disease, but both pre-clinical studies and direct human trials are underway to test the safety and efficacy of cholesterol clearing compounds, with good success already observed in animal models. Key to assessing the effectiveness of interventions in patients, however, is the development of objective neurobiological outcome measures. Multisensory integration mechanisms present as an excellent candidate since they necessarily rely on the fidelity of long-range neural connections between the respective sensory cortices (e.g. the auditory and visual systems). A simple way to test integrity of the multisensory system is to ask whether individuals respond faster to the occurrence of a bisensory event than they do to the occurrence of either of the unisensory constituents alone. Here, we presented simple auditory, visual, and audio-visual stimuli in random sequence. Participants responded as fast as possible with a button push. One 11-year-old and two 14-year-old boys with NPC participated in the experiment and their results were compared to those of 35 age-matched neurotypical boys. Reaction times (RTs) to the stimuli when presented simultaneously were significantly faster than when they were presented alone in the neurotypical children, a facilitation that could not be accounted for by probability summation, as evidenced by violation of the so-called ‘race’ model. In stark contrast, the NPC boys showed no such speeding, despite the fact that their unisensory RTs fell within the distribution of RTs observed in the neurotypicals. These results uncover a previously undescribed deficit in multisensory integrative abilities in NPC, with implications for ongoing treatment of the clinical symptoms of these children. They also suggest that multisensory processes may represent a good candidate biomarker against which to test the efficacy of therapeutic interventions.